Although a muscle contracture can feel like it comes on out of the blue, it develops over time.
Muscles grow short and tight, limiting range of motion and causing stiffness and pain. Disabled people often struggle with muscle contractures, but what are they exactly?
Types and Causes of Muscle Contracture
People living with disabilities often experience contractures as a disease worsens and attacks their bodies. Those with cerebral palsy may be more prone to the condition, but injury, nerve damage from a stroke, ageing and other chronic diseases can also lead to:
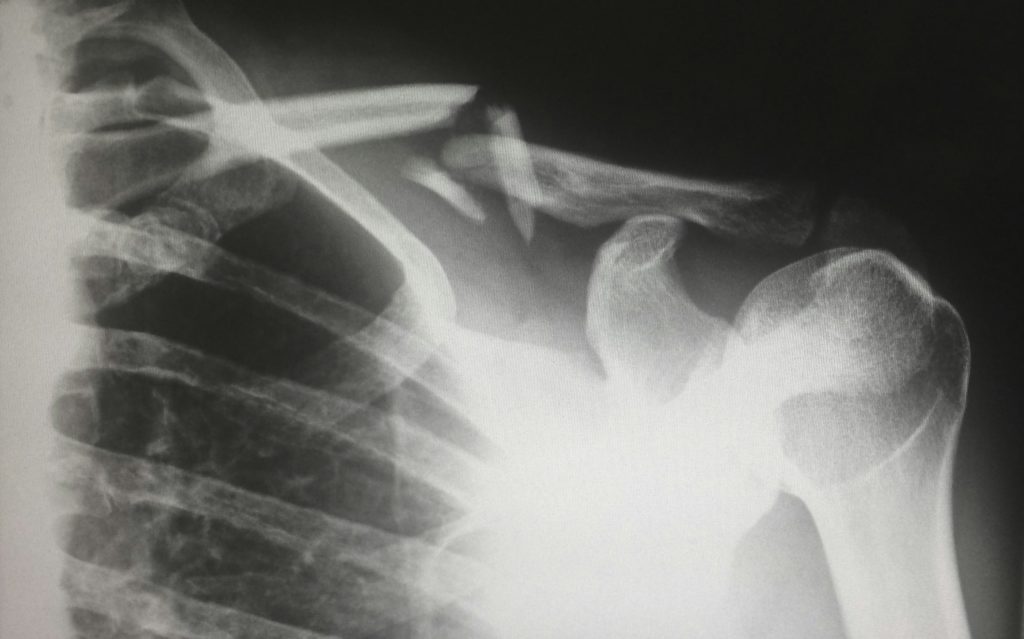
- Frozen shoulder: Often age-related or from sports injuries
- Clubfoot: Congenital condition where a foot turns awkwardly
- Dupuytren’s contracture: Seen in people with disabilities where the fingers bend toward the person’s palm
- Volmann contracture: The fingers and wrist twist and look like a claw
- Soft tissue contractures: Usually seen from injuries
- Arthrogenic: Caused by osteoarthritis and sclerosis
- Equinus: An issue with the ankle joint that can impact walking
- Myogenic: Usually from a stroke or other health concern
Understanding the causes of each type of muscle contracture allows you to work with your physician on the best treatment protocol.
What Does a Muscle Contracture Feel Like?
Some of the symptoms you’ll experience with muscle contractures may feel like overuse in the beginning. You could have:
- Loss of movement
- Pain
- Tight or stiff feeling
You may experience one or all of the symptoms, depending on the muscle contracture type you have.
What Treatment Options Are Available for Muscle Contractures?
Some treatment options exist, depending on a disabled person’s overall diagnosis and whether the contracture would come back. However, for those who qualify, options include:
- Gentle stretching to increase range of motion
- Wearing a brace or splints to keep the joint in the proper position
- Joint relaxers or nerve blockers to ease and manage pain
- Physical therapy
- Surgery
Doctors will likely try other methods before turning to surgery. One of the most common procedures involves tendon lengthening — or tenotomy. The surgeon cuts the tendon to allow for more movement and sometimes reroutes it to ensure proper muscle function.

Living With Muscle Contractures and Lessened Mobility
Managing muscle contractures is a complex endeavour. Treatment can depend upon the underlying conditions causing the muscle stiffness in the first place. Some ways the condition impacts daily life include difficulty with basic daily tasks such as eating, walking and dressing oneself.
In severe cases, the person may need 24/7 care, meaning they lose independence. The psychological toll of your body not doing as you command combined with pain and discomfort can be mentally exhausting.
With some diseases, the condition is progressive. For example, muscular dystrophy (MD) leads to fibrous tissue and fat replacing muscle and overall degeneration. A study involving 156 participants with MS found that 56% had contractures in at least one major joint of the upper or lower limb, with the ankle being the most common site (43.9%)
The key to living with lessened mobility is to treat the underlying causes as long as possible and with emerging medicine. As scientists learn more about the human body and how it functions with symbiotic internal relationships, they’re also learning better ways to treat diseases like Parkinson’s, MD and various genetic conditions.
What Can You Do Today to Reduce Muscle Contractures?
In addition to nonsurgical treatments like physical therapy, there are some things people can do to reduce muscle contractures or even prevent them in the future:
- Stretch commonly affected muscle groups, such as shoulders, glutes, hamstring, ankles and wrists, and hands. Finding stretching exercise videos on YouTube put out by licensed physical therapists can be helpful. You can also ask your doctor to refer you to a PT and learn the best motions to protect you from injury or strain.
Football Players vs. Untrained Boys: A study comparing prelavence of contractures in junior male football players compared to untrained boys found that football players had significantly better spine mobility and fewer muscle contractures, particularly in the older age groups. This is thought to be due to stretching exercises recommended as elements of warm-ups.
- Take a hot bath or place heat on the affected muscles.
- Speak to your doctor about recent research on when the best time to stretch is and how best to heat up the muscles.
- Get active, as moving around can help maintain motion range. Pay attention to your body — if something hurts, try to find a different position.
- A stroke damages your nerves and how they control muscles. Medications like muscle relaxers can also reduce muscle stiffness in the short term.
Even little changes can have some impact and reduce the muscle stiffness you’re experiencing. For people who cannot walk or participate in physical activities, having someone who knows how to stretch and lengthen muscles can prevent atrophy.
Set Personal Goals to Manage Muscle Contractures
Facing a lack of mobility can be frustrating, so look for ways to get out and do the things you love. Use a scooter if it’s difficult to walk, go out to dinner with a friend and surround yourself with the things you love. Talking to a counsellor well-versed in the psychological impact of your condition can give you additional coping tools to live a full life with less pain.
Pharmaceutical companies and scientists uncover new treatments every day. Keeping your muscles as healthy as possible until a permanent solution for muscle contractures arrives could help alleviate symptoms.
How to Prevent Muscle Contractures in Daily Life
Preventing muscle contractures involves regular movement and muscle care. Some simple steps can help maintain flexibility and prevent worsening stiffness:
- Daily Stretching: Gentle stretches targeting commonly affected muscles, such as shoulders, ankles, and wrists, can prevent tightness.
- Hydrotherapy: Water-based exercises, like swimming or hydrotherapy pools, can ease joint stiffness and improve mobility.
- Use of Splints and Braces: These help maintain a correct position and prevent further muscle shortening.
- Physical Therapy: A physiotherapist can create a stretching and strengthening plan tailored to your needs.
- Assistive Technology: Devices such as adaptive seating and supports can provide comfort and mobility support.
- Nutrition and Hydration: Eating a balanced diet rich in anti-inflammatory foods and staying hydrated supports muscle health.
- Regular Medical Check-Ups: Consulting a specialist can help monitor muscle contractures and adapt treatment plans.
Taking proactive steps can make daily life more comfortable and reduce the risk of severe muscle contractures over time.
Check out our range of mobility aids for support with movement and posture.
About the Author: Duncan Edwards
Living with and caring for a disabled family member has given me firsthand experience with muscle contractures and their impact on daily life. From attending medical appointments to working alongside physiotherapists and carers, I’ve navigated the complexities of managing stiffness, pain, and mobility challenges. Through my work with Disability Horizons Shop, I’ve helped provide practical solutions for disabled people, ensuring greater independence and comfort. I’m passionate about sharing trusted, practical advice to support others in living life to the fullest, no matter the challenges they face.